Breastfeeding during a Pandemic
Key Messages
• An increased rate of breastfeeding cessation has been observed in many countries during the pandemic.
• Breastfeeding should be supported in all mothers with a SARS-CoV-2 infection who are able to take care of their offspring.
• Maternal vaccination against SARS-CoV-2 is safe for the offspring and might further strengthen the protective role of breastmilk against viral infections
Abstract
Background: The current pandemic and the concerns of vertical transmission of SARS-CoV-2 have contributed to increasing the rate of breastfeeding interruption. This tendency has been associated with negative effects on the well-being of lactating mothers and their infants. The aim of this review is to summarize the evidence on the strategies to support breastfeeding during the COVID-19 pandemic and on the safety of breastfeeding during a SARS-CoV-2 infection or after COVID-19 vaccination.
Summary: Available data show that the lack of support of lactating mothers during the pandemic has contributed to breastfeeding cessation worldwide. However, a few strategies have been proposed to overcome this issue. The risk of SARS-CoV-2 transmission from infected mothers to their offspring is extremely low. Furthermore, vaccination of lactating mothers is not associated with side effects in their infants.
Key Messages: Increasing effort should be made to support breastfeeding during the COVID-19 pandemic. Mothers who are able to take care of their offspring and to adopt basic hygiene measures should not interrupt breastfeeding during a SARS-CoV-2 infection. Vaccination of lactating mothers might further strengthen the protective effect of breastfeeding against infections.
Introduction
Breastfeeding and Previous Pandemics
Scientific historiography on breastfeeding is relatively recent and the first documents are available from 1476 [1]. Although maternity clinics were created earlier (Fig. 1), breastfeeding has received an increasing attention by scientists only from the 19th century onwards.
Breastfeeding has traditionally been considered as a beneficial practice also during diseases [2]; however, few documents specifically addressed the issue of breastfeeding during pandemics. In 1832, a publication on cholera-morbus reported that the disease did not prevent the possibility of breastfeeding even in severely affected mothers [3]. A further case study noted that lactating women were at lower risk of death from cholera infection as compared to nonlactating mothers [4]. Similar observations were also made during the “Spanish flu” pandemic [5]. The possible risks associated with breasfeeding were only widely addressed during recent infectious emergencies (e.g., HIV).

The COVID-19 Pandemic as a Natural Disaster
The COVID-19 pandemic has impacted the lives of the world's population. In terms of the number of deaths, hospitalizations, and consequences on social life and economy, this global crisis could be equated to natural disasters. In these circumstances, some categories of people are defined as “vulnerable” or “at risk” and should obtain dedicated support. Among these, newborns and their mothers can undoubtedly be defined as a vulnerable population. The overload of health workers with the consequent reduced availability for care, the need for social distancing and even isolation of mothers, and the difficulty of finding reliable scientific information are only a few of the issues that are impacting the mother-child dyad.
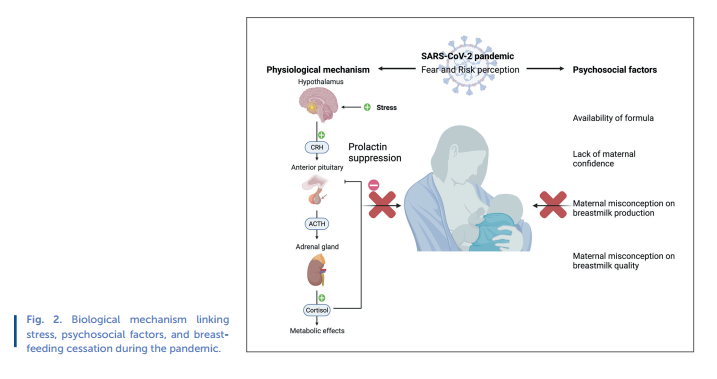
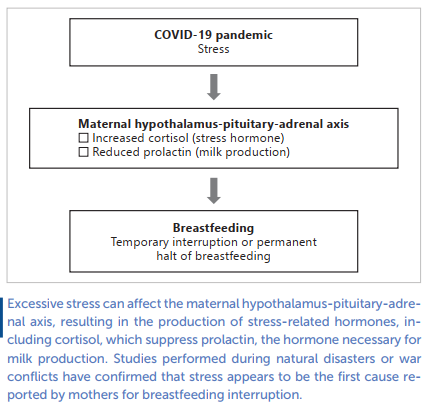
It is also known that mothers exposed to a catastrophic event are at greater risk of prematurely terminating breastfeeding [6]. This is due to a biological mechanism linked to excessive stress and some psychosocial factors (Fig. 2). The maternal hypothalamus-pituitary-adrenal axis is overstimulated to release the so-called stress-related hormones, including cortisol, which in turn suppresses prolactin, the hormone necessary for milk production [7]. Recent studies carried out during natural disasters or war conflicts have confirmed that stress appears to be the first cause reported by mothers for breastfeeding interruption [8, 9]. The increased availability of formula milk given by charities, misconceptions about milk production, lack of maternal confidence during breastfeeding, and the concern of vertical transmission of SARS-CoV-2 have likely played a negative role on breastfeeding [10, 11]. Therefore, there is an urgent need to provide evidence-based information and support to lactating mothers.
The aim of this review is to summarize evidence on the following three topics: (1) the support of breastfeeding during the COVID-19 pandemic; (2) breastfeeding during a SARS- CoV-2 infection; and (3) COVID-19 vaccination in lactating mothers.
Support of Breastfeeding during the COVID-19 Pandemic
In the last decades, breastfeeding has been supported by many authorities, including the WHO, which recommends exclusive breastfeeding for the first 6 months of the baby's life [12]. During the COVID-19 pandemic, breastfeeding takes on even greater importance for both mother and baby. It is known that breastfeeding is a protective factor for the mother against postpartum stress and depression development. A recent study by Dagla et al. [13] confirmed that breastfeeding and its duration could positively influence maternal mental health, demonstrating how a shorter duration of breastfeeding is related to symptoms of psychological distress, initiation of psychological therapy, and higher scores on the Edinburgh Postpartum Depression Scale. Previous studies have obtained similar results, confirming the association between breastfeeding and maternal mental health [14]. Given the increased risk of mental health issues during a pandemic, both in the general population [15] and especially in mothers [16], it is clear that breastfeeding is of fundamental importance for maternal well-being during this pandemic. Breastmilk is also known to have a strong immune value. It contributes to the development of the newborn's immune system and contains several substances with a marked antiviral activity [17]. For some of these substances (Table 1), such as lactoferrin and human milk oligosaccharides, the antiviral activity has been attributed such a great importance that they have been supplemented to support immunity and provide antiviral protection of adult individuals [18, 19].
The Difficulties in Promoting Breastfeeding during a Pandemic
Some authors investigated the consequences of the CO-VID-19 pandemic on nursing mothers. A work by Lucas and Bamber [20] identified the factors that place pregnant and postpartum women at greater risk of having an inadequate outcome during a pandemic: (1) reduced access to antenatal and postnatal care; (2) lack of in-person clinical evaluations; and (3) lack of screening for physical, psychological, and social issues. A study conducted in the UK found that in 27% of women, lockdown and lack of support led to early termination of breastfeeding [21]. A review by Pacheco et al. [22] confirmed that when mothers struggled with breastfeeding and perceived decreased family and professional support, they were at risk of mental health problems. The change of hospital policies in some countries, with the introduction of social distancing and the inability of the father to be with the mother in the immediate postpartum period, also represents a significant risk factor for maternal mental problems. A study conducted in Italy showed that mothers who were forced to be separated from their partner showed a higher rate of anxiety and had a worse perception of the support received from the staff [23].
Possible Strategies for Breastfeeding Protection and Promotion
To overcome these crucial issues that can affect the prevalence and duration of breastfeeding, some authors have proposed intervention plans and new ways to ensure the necessary support of mothers. A review by Lubbe et al. [24] collected the indications of the leading world organizations and scientific societies, emphasizing the importance of not separating the mother and the child even in maternal illness. Furthermore, in the case of compromised clinical conditions or maternal malaise, the importance of continuing breastfeeding is emphasized, inviting the mother to express the milk and give it to the child, given the low risk of viral transmission through breast milk. A large multicenter study has also confirmed that rooming-in is feasible and recommended even for mothers hospitalized with a nonsevere form of COVID-19, with evident benefits on the initiation and maintenance of breastfeeding [25]. A survey conducted in Spain by Munoz- Amat et al. [26] described well which standards of care relating to childbirth and the postpartum period have been changed due to the pandemic. However, the same authors have shown how the structures committed to the UNICEF Baby-Friendly Hospital Initiative (BFHI) managed to guarantee standards of care and procedures similar to those before the pandemic and provided better support for mothers with and without COVID-19. In addition to ongoing and unchanged support from health professionals, some authors have suggested new ways to ensure adequate help for nursing mothers during a pandemic [27, 28]. Telemedicine has been adopted to improve support for pregnant women in managing peculiar situations, such as gestational diabetes or weight gain [29]. Given these promising results, it would be desirable to make greater use of some existing platforms to support nursing mothers by qualified personnel [30]. Adequate prenatal training on breastfeeding can also be successfully conducted electronically [31]. A review by Singh et al. [27] has summarized some of these innovative strategies, which are able to reach mothers even in rural or particular contexts and which appear to be an up-and-coming tool for the promotion and protection of breastfeeding in times of pandemic.
Breastfeeding during a SARS-CoV-2 Infection
Since the onset of the pandemic, the safety of breastfeeding has been debated worldwide, and not all authors agree on the management of the infant-mother dyad [32, 33]. The following three scenarios might occur in day-to-day clinical practice: (1) a lactating mother affected by COVID-19 and an infant testing negative for SARS-CoV-2 infection; (2) both a lactating mother and her infant affected by SARS-CoV-2 infection; and (3) only the breastfed infant testing positive for SARS-CoV-2. These three scenarios deserve some discussion.
Four rather large studies conducted in high-income countries reached similar conclusions about breastfeeding of healthy infants by mothers with a SARS-CoV-2 infection. Ronchi et al. [25] prospectively evaluated 60 neonates and one pair of twins born to 61 mothers with SARS-CoV-2 infection in a multicenter study conducted in Northern Italy. None of the included neonates presented a positive SARS-CoV-2 test at the enrolment. There was rooming-in and breastfeeding together with systematic implementation of physical distancing (2 meters) of mothers and infants except for breastfeeding and routine care that could be done by mothers wearing a surgical face mask and after handwashing. At discharge (median 5 days after delivery), only 1 neonate presented a nasal swab positive for SARS-CoV-2. A retrospective study conducted by Dumitriu et al. [34] in two hospitals in New York found that among the 91 breastfeeding mothers with a positive test for SARS-CoV-2 infection, no evidence of vertical transmission was found. Of note, among the mothers included in the study, 76 were roomed-in with their neonates.
In a study carried out by Shlomai et al. [35] in Israel, 41 neonates born to mothers with a SARS-CoV-2 infection were separated from their mother till discharge but received ex-pressed unpasteurized breastmilk. None of the neonates presented a positive SARS-CoV-2 test at 14-21 days of life. Finally, a multicenter cohort study conducted in Massachusetts [36] followed up 255 newborns of mothers with a SARS- CoV-2 infection during the hospital stay and for a further 30 days. The mother-infant dyad was not separated. Among the 6 infant cases with a positive SARS-CoV-2 test during the follow-up, only 2 were breastfed.
A prospective cohort study including 263 infants in USA [37] specifically focused on the clinical course of infants (e.g., development of respiratory infections) born to mothers affected by SARS-CoV-2 versus those unaffected. Most included infants (>85%) were breastfed during the study. The authors found no differences in clinical outcomes of infants 6-8 weeks of age born to mothers with and without SARS-CoV-2 infection.
Further smaller case series have investigated the possible transmission of SARS-CoV-2 through breast milk, and all concluded that the risk of vertical transmission was very low [24].
Cases of infant-lactating mother dyads both concurrently affected by SARS-CoV-2 have been reported in anecdotal reports [38, 39]. In almost all published cases, the infant's clinical course was mild or even uneventful. On the other hand, only 1 case of an infant affected by SARS-CoV-2 and breastfed by an uninfected mother has been published. The infant presented a mild disease and the mother never developed symptoms nor presented a positive test for SARS-CoV-2 [40].
Data from clinical observations are consistent with findings of laboratory studies. A recent meta-analysis analyzed reports investigating the presence of the SARS-CoV-2 genome in human breast milk of mothers with a SARS-CoV-2 infection [41]. The study identified a total of 183 (49%) mothers with a SARS- CoV-2 infection whose breastmilk was also tested for the presence of the SARS-CoV-2 genome. Furthermore, the presence of immunoglobulins (Ig) against the virus was tested in the breastmilk of 89 out of the 183 infected mothers. Twelve mothers were positive for the presence of SARS-CoV-2 in the breast milk. Six out of the twelve mothers with SARS-CoV-2 in the breast milk tested positive for a SARS-CoV-2 infection. Among these 6 infants, 4 were symptomatic and only 1 re-quired ventilatory support. On the other hand, this infant tested positive also for a respiratory syncytial virus [42]. A total of 30 (16%) mothers presented Ig against the virus without SARS- CoV-2 genome in their breast milk. Overall, these data confirmed that the risk of SARS-CoV-2 vertical transmission through breast milk is very limited and the risk of severe infection for breastfed infants of mothers affected by SARS-CoV-2 is even lower.
Another recent systematic review has synthetized available recommendations for breastfeeding mothers affected by SARS-CoV-2 [43]. The review identified 73 articles reporting recommendations (including guidelines) on this issue. Most articles both supported direct breastfeeding and hygiene preventive measures comprising, among others, handwashing, face masks wearing, and regular breast cleaning, in cases without any other contraindication concerning breastfeeding. Although a few authors recommended expressed breast milk in case of symptomatic mothers or even separation of the infant, many international authorities, including the WHO, the International Federation of Gynecology and Obstetrics, and the Royal College of Obstetricians and Gynecologists, are in favor of direct breastfeeding (along with hygiene precautions) except for mothers who are too sick and unable to care for their offspring [44, 45]. The latter approach is further supported by emerging evidence on the presence of neutralization antibodies in human milk from COVID-19-infected mothers [46, 47].
Breastfeeding and COVID-19 Vaccination: How Far Have We Come?
Data on the efficacy and safety of COVID-19 vaccination while breastfeeding are scarce since breastfeeding women were excluded from the clinical trials of COVID-19 vaccines [48]. Taking into account the limited knowledge on the effects of vaccines either on the infant or on the milk production and excretion, concerns have therefore been expressed on the risks of vaccination in the breastfeeding population potentially outweighing the benefits [49]. As a result, even though the WHO does not recommend against vaccination during breastfeeding [50] and several other health authorities have not issued a true contraindication, highlighting the lack of scientific data, breastfeeding women may be potentially challenged by the choice between continuing to breastfeed or postponing vaccination [51].
Accordingly, a low COVID-19 vaccine acceptance among breastfeeding women has recently been reported by Sutton
et al. [52]. The authors have conducted an online survey including 1,012 women, among whom 216 were pregnant and 122 were breastfeeding, and found that breastfeeding respondents were less likely to accept vaccination as compared to nonpregnant women (55.2 vs. 76.2%, p < 0.001). The most frequent reasons reported for declining vaccination were the lack of confidence in medical authorities and misconceptions regarding vaccination safety and side effects. These results highlight the need for spreading more information and education on these issues in order to promote an informed decision about COVID-19 vaccination among breastfeeding women.
Protection of COVID-19 Vaccination for Lactating Mothers and Their Infants
Previous experience with other vaccines (e.g., influenza and pertussis) administered during pregnancy clearly indicates that vaccination provides protection both to the mother and the infant [17]. Besides transferring maternal antibodies to the infant, human milk further provides huge amounts of bioactive components, thus contributing to the infant's protection against the pathogens that can be encountered in the surrounding environment [53].
While available evidence does not support the transmission of SARS-CoV-2 through breast milk [54], it has been demonstrated that the milk produced by infected mothers is a source of anti-SARS-CoV-2 IgA and IgG antibodies and has a high neutralizing antiviral activity, thus contributing to the infant's protection against infection [55]. Since vaccination has become widely available, attention has focused on the investigation and quantification of specific anti-SARS-CoV-2 antibodies in milk after maternal vaccination.
Low at al. [56] enrolled 14 breastfeeding health workers who had received two doses of the BNT162b2 vaccine, with the second dose administered on day 21. The authors reported that in breast milk collected within 3-7 days after the second dose of vaccine, SARS-CoV-2-specific IgA and IgG were detected in 86% and 100% of the recruited mothers, respectively. The reported values at that study point were significantly higher than those found at the two previous time points (1-3 days after dose 1 and 7-10 days after dose 1), indicating that the strongest antibodies response to vaccination was induced within 3-7 days after the second dose. The virus-specific IgG titers did not significantly decrease through the 4-6 weeks following the second dose, whereas the virus-specific IgA concentrations concomitantly decreased. These results suggest a time-dependent increase of the IgG/IgA ratio, consistent with the data reported after respiratory syncytial virus infection [57]. Remarkably, a limited amount of vaccine mRNA has been detected in few milk samples, suggesting its minimal transfer. However, infants who were fed postvaccination breast milk during the following month did not show any adverse effect, further supporting the safety of vaccination among breastfeeding women. Contrary to these findings, Golan et al. [58] did not detect the presence of vaccine-associated mRNA in 13 milk samples collected 4-48 h after vaccination from 7 breastfeeding mothers. Moreover, it is acknowledged that any nanoparticles from currently available COVID-19 vaccines potentially ingested by the breastfed infant would be destroyed during the gastrointestinal passage, thus without being absorbed [59].
Perl et al. [60] have also detected the presence of anti- SARS-CoV2-specific IgA and IgG antibodies in a large cohort of 84 breastfeeding women who had received two doses of the BNT162b2 vaccine. The authors confirmed the passage of IgA antibodies into breast milk already at 2 weeks after the first dose, with the sharpest increase 1 week after the second dose. Concentrations of anti-SARS- CoV-2-specific IgG were low in the first 3 weeks after the first dose but increased significantly after the first week following the second dose and remained high even in the following 2 weeks. Esteve-Palau et al. [61] further reported that, after the second dose of vaccine, the anti- SARS-CoV-2 IgG detected in the breast milk of the 33 enrolled lactating women were positively correlated with maternal serum concentrations. Recent evidence suggests that the titers of anti-SARS-CoV-2-specific IgA and IgG detectable in breast milk may differ according to the type of vaccination administered to the lactating women. Lechosa-Muniz et al. [62] analyzed the milk samples of 110 breastfeeding mothers and found higher levels of antibodies, both in serum and breast milk, from mothers vaccinated with BNT162b2 or mRNA-1273 vaccine as compared to ChAdOx1-S.
Impact of COVID-19 Vaccination on Lactation
McLaurin-Jiang et al. [48] conducted a cross-sectional survey of 4,455 lactating women following COVID-19 vaccination with the aim of investigating the occurrence of vaccine-related side effects that could negatively impact on breastfeeding. The authors found that breastfeeding mothers' vaccination was associated with only minimal disruption of lactation or adverse effects on the breastfed infants. In line with these findings, Lechosa-Muniz et al. [60] also reported that vaccines were well tolerated by the breastfeeding mothers and their infants.
Conclusions
During the current COVID-19 pandemic, most evidence highlights the importance of breastfeeding. This practice should be supported also in case of mothers affected by a SARS- CoV-2 infection who are able to take care of their offspring and to adopt basic hygiene measures. Pasteurization of breast milk is not necessary, and the interruption of breastfeeding is both not recommended and potentially harmful for the well-being of mothers and infants. Finally, Ig anti-SARS-CoV-2 in breastmilk following vaccination are not associated with side effects, thus strengthening the protective role of breastfeeding against viral infections.
Conflict of Interest Statement
The writing of this article was supported by Nestlé Nutrition Institute and the authors declare no other conflicts of interest.
Author Contributions
Gregorio P. Milani, Alessandro Porro, and Maria Lorella Gianni wrote the first draft of the manuscript. Carlo Agostoni supervised and critically reviewed the manuscript and gave a significant contribution in his field of expertise.
References